Phone 248.871.7756 | Email info@gmedicareteam.com
Watch Videos on 
 Search
Search

Take a full 16 minutes to watch the video below and please make sure to pay attention. As you are observing the video, write down any additional questions that come up in your mind so you can have them answered during your enrollment process. The selection of either Medigap or Medicare Advantage is one of the most difficult decisions seniors have to make when they start their journey with Medicare.
BONUS - if you refuse to spend the full 16 minutes, please at least watch the 10 minute version below it! Commit a little bit of time, please.
Once you have made the decision that you need to sign up for Medicare part A and Part B, it is time to decide how you fill the financial holes present in original Medicare. It is important to note that this discussion will not include retiree coverage from a former employer, the government, or through military service. If you do not plan on receiving retiree benefits, you will have to turn to the private market to find the best plan to fit your healthcare needs. This Article will help you learn how each product type works, Medigap Vs. Medicare Advantage.
There are two main ways to receive additional coverage when you are Medicare eligible. The first is Medigap (sometimes referred to as a Medicare supplement). The second option is Medicare Advantage (often referred to as Part C or MA plans).
Medigap plans are offered by private insurance companies as secondary insurance to fill in the “gaps” that are left by original Medicare (ex. the 20% part B coinsurance). To learn even more details about Medigap plans, watch this video.
Medicare Advantage plans, on the other hand, are offered by insurance companies as private alternatives to original Medicare. These plans typically include additional benefits to Medicare such as dental/vision/hearing coverage, prescription coverage, over the counter benefits and no-cost gym memberships. In exchange for these benefits, enrollees agree to see medical providers in the insurance companies contracted network (typically smaller than original Medicare). We have created a video explaining Medicare Advantage plans.
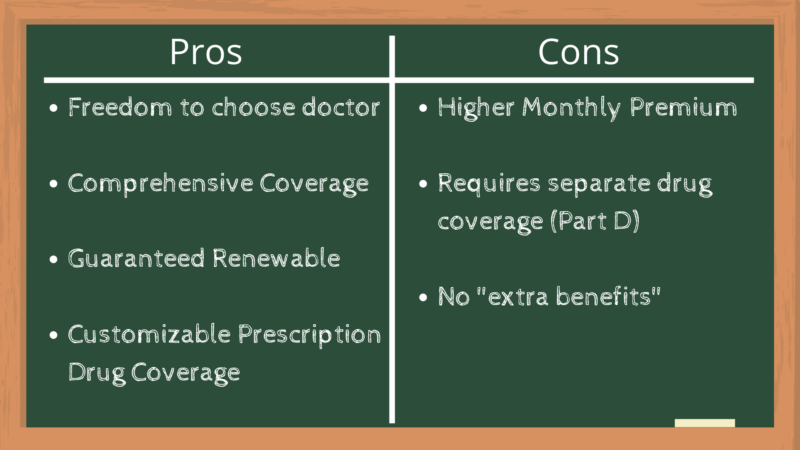
Now that we have covered the main difference between the two options, we will highlight the main pros and cons of both. Let’s start by taking a more in-depth look at Medigap plans.
Freedom to choose your doctors // One of the key features of Medigap plans is that they are secondary insurance compared to original Medicare. If you have a Medigap plan, you can go to any doctor or hospital that accepts Medicare’s assignment. By law, if a provider accepts Medicare, they also must accept your Medigap plan (regardless of the insurance company that provides your coverage). Having nationwide coverage can be crucial if you plan to travel around the country or simply if you want access to the best care from top-rated facilities around the country.
Comprehensive medical coverage // Aside from your monthly premium, Medigap plans come with very little out of pocket costs when you receive medical care. The most popular Medigap plan (Plan G) covers all out of pocket costs after you pay the yearly deductible of $257 (provided your procedures are approved by Medicare). Another benefit to having lower out of pocket medical costs is that budgeting health care expenses can be much easier.
Medigap contracts are guaranteed renewable // “Any standardized Medigap policy is guaranteed renewable, even if you have health problems. This means the insurance company can’t cancel your Medigap policy as long as you pay the premium." - Medicare.gov.
Medigap plans require separate drug coverage // Now we know what you’re thinking, how is needing separate drug coverage a good thing? We will admit this is both a positive and negative when it comes to Medigap coverage. The reason this can be positive is that it allows you to customize your insurance options. This means that you can choose the Medigap plan that best fits your situation, while also choosing a drug plan that best fits your specific prescriptions. This also means that during the Annual Election Period (AEP) in the fall, you can change your prescription coverage without impacting the coverage of your Medigap plan.
Higher monthly premiums // On average, Medigap plans come with higher monthly premiums than Medicare Advantage plans. For example, someone turning 65 in Michigan can expect to pay around $140/month. Compare this to Medicare Advantage plans that are commonly available for $0/month.
Medigap plans require separate drug coverage // We weren’t kidding when we said this a positive and a negative to having Medigap coverage. Having separate part D coverage comes with added premiums, as well as added complexity. The average premium for part D in 2025 is $46.50/month. This monthly cost is in addition to the roughly $140/month for a Medigap plan G. Prescription drug coverage (part D) is usually provided by a different insurance company than your Medigap plan. This means you will have more coverage to keep straight and we all know that Medicare can already be confusing enough.
No additional benefits // Medigap plans typically do not include prescription coverage, dental/vision/hearing coverage, or gym memberships. It is easy to buy separate insurance for dental/vision/hearing but it does come with added costs.
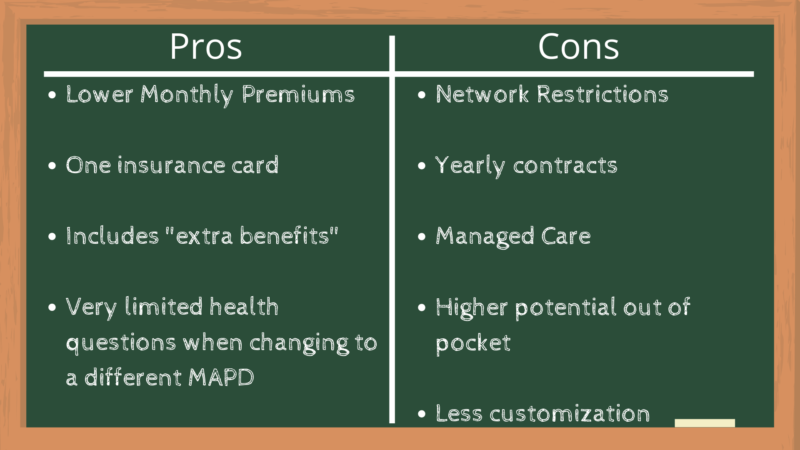
Lower monthly premiums // The national average premium for Medicare Advantage plans in 2025 is $17.00/month according to the Centers for Medicare & Medicaid Services (CMS). However, as we mentioned before, there are many Medicare Advantage plans across the country that are $0/month.
Single Insurance Plan // Medicare Advantage plans are often seen as a more convenient choice for Medicare coverage. The bundled approach of Medicare Advantage plans means that you can use the same insurance coverage/card at both the doctors and the pharmacy. Although this is often seen as a benefit to Medicare Advantage coverage, we highly recommend that you do not make this the reason you do, or do not choose one option over the other.
Additional Benefits // Unlike with Medigap plans, Medicare Advantage plans commonly include dental/vision/hearing coverage, gym memberships and prescription drug coverage at no added cost.
Limited discrimination for pre-existing conditions // The only medical disqualifier for enrolling in a new Medicare Advantage plan is if you have end-stage renal disease (ESRD). For individuals with many ailments, this means they can change Medicare Advantage plans during the proper enrollment periods as long as they do not have ESRD.
Limited Networks // Medicare Advantage plans commonly come in the form of HMO’s and PPO’s (click here for a detailed description of the two). If you have a Medicare Advantage plan you will typically have to healthcare providers in the plans contracted network, or you will likely have much higher out of pocket costs. Restricted networks place an increased burden on individuals that enjoy frequent travel, or anyone that wants unrestricted access to premier medical facilities nationwide (or even state-wide).
Yearly contracts // Medicare Advantage plans are renewed on a year-to-year basis. Medicare Advantage plan benefits typically change every year, which can cause either negative or positive impacts for enrollees (created increased uncertainty in retirement). Perhaps the biggest con to having a yearly contract is that your doctors are not under the same contract constraints. Doctors and even entire health systems can cease their contract with a Medicare Advantage plan at any time of the year. Meanwhile, enrollees in the plan do not have the same luxuries. If your doctor or hospital stops accepting a plan mid-year, you will have to find alternatives or pay higher out of network costs until you can make a change during an enrollment period.
Managed Care // The best way to describe managed care is by quoting PBS Medicare contributor, Phillip Moeller, “One reason MA plans can offer more benefits and often charge less is that they can save money on medical expenses through their business agreements with members of their provider networks. The bigger source of savings, however, is that MA plans are managed care plans. Original Medicare is what’s called a fee-for-service program. If you want a procedure that Medicare approves, it will be covered by original Medicare. MA plans, by contrast, would look for low-cost providers of such procedures. They usually require enrollees to get pre-authorization from their plan before approving coverage and may require less-expensive treatment alternatives.”
Essentially, Medicare Advantage plans will take a more “active” role in your healthcare. Getting approval for certain higher-cost procedures can become a hassle at unfortunate times.
Higher out of pocket costs for medicare care // Medicare Advantage plans typically come with a lower monthly premium than Medigap plans, but in exchange, they also come with higher out of pocket costs when you seek medical care. Medicare Advantage plans can have a maximum out of pocket (MOOP) of up to $8,850 with most plans having a MOOP of approximately $5,000/year. Also, prescription drug costs do NOT count towards the maximum out of pocket. Overall, this makes budgeting with Medicare Advantage plans much more difficult than with Medigap plans.
Less flexibility with coverage options // The bundled “one size fits all” style of Medicare Advantage plans can make it difficult to find the plan that best fits your unique needs. It can become difficult to find a plan that covers all of your medications perfectly while having all of your doctors in the network. Typically, this becomes more of an issue for individuals with more healthcare needs and ailments.
This is by far the most important part of this entire article, so hopefully, you have stayed with us until this point. Deciding between a Medicare Advantage plan or a Medigap plan is likely the most important decision you will make signing up for Medicare.
The reason the decision is so important is that when you first enroll in Medicare part B, you start your Open Enrollment Period (OEP). The OEP is specific to you! This has nothing to do with AEP in the fall, which is commonly incorrectly called “open enrollment”. Your Open Enrollment Period starts 6 months BEFORE you start part B and lasts for 6 months AFTER you start part B. Again, this is when you first enroll in part B of Medicare (even if you wait until age 80 to do so) and not when you turn 65.
During your Open Enrollment Period, you can purchase ANY Medigap plan on the market and NOT have to answer health questions. You could have a terminal disease and still be automatically accepted by a Medigap plan during this period. After your Open Enrollment Period, if you want to change Medigap coverage, you will have to answer health questions (go through underwriting) to qualify for the Medigap plan. If you do not answer “no” to all the health questions there is a very good chance you will be DENIED from getting new Medigap coverage. This also applies to anyone changing from a Medicare Advantage plan to a Medigap plan.
Medigap Open Enrollment is a very important topic, so click Here to learn more. The moral of the story is that when you first start part B of Medicare, please make sure to look at every option and choose a plan style that you are comfortable with for potentially decades to come.
Fill out the form here and someone will be in touch soon.