Phone 248.871.7756 | Email info@gmedicareteam.com
Watch Videos on 
 Search
Search

 Tom lost his job at age 67. When he worked with his HR department, they gave him documents to secure coverage via Cobra. While this could be a good option for Tom, no one told him that if he starts Cobra coverage, he would need Medicare as well…..
Tom lost his job at age 67. When he worked with his HR department, they gave him documents to secure coverage via Cobra. While this could be a good option for Tom, no one told him that if he starts Cobra coverage, he would need Medicare as well…..
Tom was reading through the paperwork for Cobra when he went back to HR the next day and asked for more information about Medicare and penalties possibly related to Cobra? He was extra concerned about having continuous coverage since his wife was live through a pretty horrible health ordeal and requiring frequent doctor and hospital visits. All while he had to make some pretty significant decisions about their coverage.
The human resources department referred them to us to answer some Medicare questions.
Tom and his wife had done all the right things until this point. Since he worked for a large employer (over twenty employees) and they were both covered through the workplace health insurance, he and his wife elected to only enroll in Medicare Part A and defer Part B. That was the right thing to do.
Now, he’s lost his job. It was explained to him that the Cobra coverage was the same coverage that they’d had all of these years and he would have the opportunity to “take it with them” if that made sense.
There’s nothing inherently wrong with Cobra coverage. Where the problem arises is with the “primary payer” rules of Medicare.
When Tom was actively working and on his group insurance plan, the services that his wife was having billed was being billed (properly) the group health insurance plan. They were the primary payer and since she had Part A coverage, during any hospital stay she would get a bit of extra coverage through Medicare as they paid second in line to the group plan.
Cobra is a different story. As soon as Tom and his spouse were technically being covered under the Cobra coverage, Medicare becomes the primary payer.
So, please follow this next part carefully.
Since Tom’s wife was now covered with Cobra, she had to visit the doctors for an infusion. The infusion cost is $13,000 per treatment.
Remember that Medicare (and this would be Medicare Part B) is the primary payer. Remember that she and Tom only had enrolled into Medicare Part A at age 65. They have no Part B. They have no primary payer. The Cobra plan can technically pay 20% of the infusion charge as they are only required to pay as the secondary payer.
What did we do? We helped Tom and his wife hustle to get the Part B coverage retroactive to the first of the month so that they had Cobra plus Medicare and won’t have billing issues.
We then evaluated the cost and coverage of Cobra vs that of Medicare Part B and a Part D plan.
We enrolled them both into Medigap and a Part D plan for the following month. They spent only one month on the higher priced (and poorer coverage) Cobra insurance plan.
If you or anyone you know is leaving a job post age 65, please be sure they or you talk to someone about the implications that Medicare can bring to their situation.
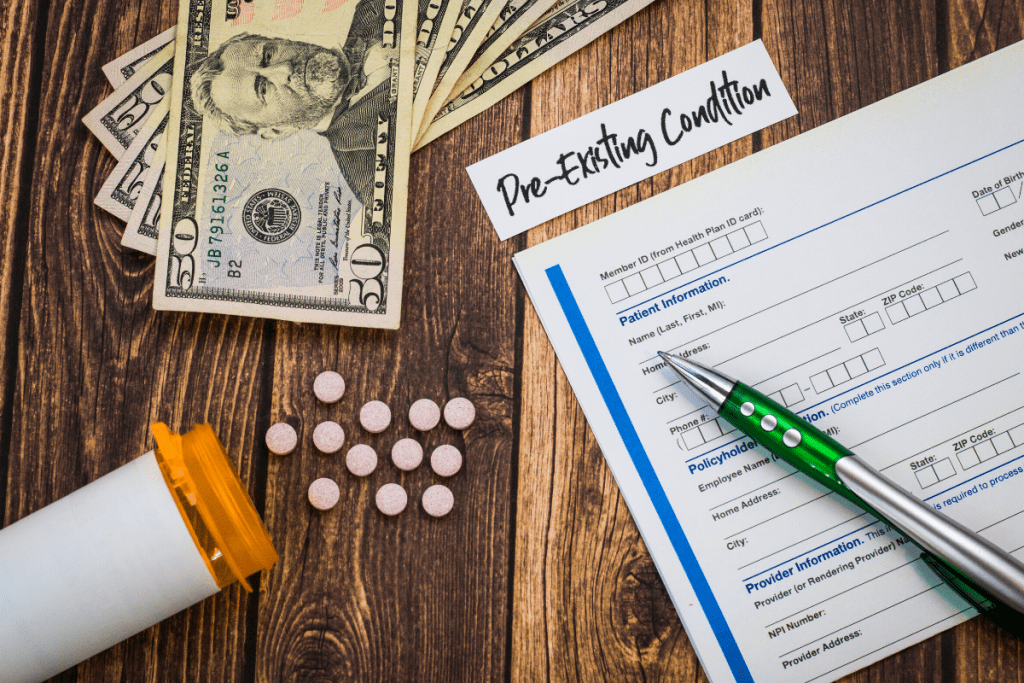 Bonnie started Medicare at age 65. She purchased a Medicare Advantage plan with her local agent who only presented coverage options based on her current health. A few years later she was diagnosed with cancer and then wanted to understand her insurance options; only to realize they were limited….
Bonnie started Medicare at age 65. She purchased a Medicare Advantage plan with her local agent who only presented coverage options based on her current health. A few years later she was diagnosed with cancer and then wanted to understand her insurance options; only to realize they were limited….
Here in Michigan, one of our local carriers has verbiage on their website posing the question “are you a light, medium or heavy user of health insurance?? The answer to your questions is intended to guide you into the proper plan.
Well, it might not be a bad place to start a discussion, but we find there’s much more to it.
Bonnie’s agent helped her choose a plan based on her being a light user of health insurance as she was turning 65. She took no medications and visited the doctors a couple of times a year for a physical and an annual skin check.
Three years later, Bonnie attended one of our sessions about Medicare. We spend lots of time discussing that fact that there are two paths to choose with Medicare products and the paths are rather different from one another. It’s important to understand how they work as you begin your Medicare years.
Bonnie called a few days later saying that she’d never heard of Medigap as a product. She wanted to see if she could qualify to purchase the plan. She could not.
Bonnie was diagnosed with cancer a year prior. She grew to dislike her Medicare Advantage plan with the co-pays she experienced with chemotherapy, testing and surgeries. She liked the idea of being able to see any specialist that accepted Medicare vs having to stay in her current network of physicians.
Basically, as Bonnie started to USE her health insurance, she didn’t feel that it was the best plan for her. Remember the low, medium, high question?
To this day, Bonnie does not qualify for a Medigap plan though we look at things annually.
Bonnie was frustrated that when she made her initial product selection with Medicare at age 65, she didn’t feel that she was presented two options. And, importantly, she didn’t feel that she was clearly made aware that she should her health change her status of “low user” to “high user”; she would not be able to purchase Medigap.
We introduce you to Bonnie so that you are sure to take adequate time to learn about your TWO product choices. Use the time to think down the road, understand how Medigap works, and understand how Medicare Advantage plans work. (note that Medigap is also referred to as Medicare supplements as they will supplement Original Medicare).
We find that when people truly understand their options; they tend to make better long term decisions.
 Upon retiring at age 70, Dan wanted to use his Medigap open enrollment period to choose a good plan for his retirement. However, he had unnecessarily enrolled in Part B at age 65 while he was still working. This mistake would lead to limited plan selection for him going forward, not what he intended.
Upon retiring at age 70, Dan wanted to use his Medigap open enrollment period to choose a good plan for his retirement. However, he had unnecessarily enrolled in Part B at age 65 while he was still working. This mistake would lead to limited plan selection for him going forward, not what he intended.
The Medigap Open Enrollment Period (OEP) is the 6-month period that begins on the first day of the month that you are BOTH 65 or older AND enrolled in Medicare Part B. Your Medigap OEP is unique to you, the individual and does not occur again, once it lapses. This should not be confused with the Annual Election Period (AEP) from October 15th – December 7th (which happens for all consumers enrolled in Medicare).
In Dan’s case, his Medigap Open Enrollment began the month he turned 65 (because he chose to enroll in Part B) and ended six months later, even though he never enrolled in a Medigap plan. That 6-month window was Dan’s opportunity to enroll in any Medigap plan he was eligible for in the Metro Detroit area, without health questions or the possibility of being denied coverage due to pre-existing conditions. Now, Dan was forced to either qualify for a Medigap plan through health underwriting or choose from a more limited amount of plans using his guarantee issue rights(learn more HERE)
The reason we use Dan as a case study is that his situation was 100% avoidable. He was covered by creditable health insurance provided by his large employer (over 20 employees), meaning that he was not at risk for a Part B penalty if he chose to delay his enrollment until his later retirement that he was planning.
In addition, to be an avoidable mistake, this is ended up costing Dan thousands of dollars of mostly unnecessary Part B premium. Because Dan’s employer had over 20 employees, it was the primary payer compared to Medicare. Having coverage through his employer meant that Medicare Part B premiums for secondary insurance that he was hardly utilizing since he is relatively healthy and rarely visited the doctors. As you may already know, the base rate for Medicare Part B in 2020 is $144.60/month. Over five years, this adds up to be a substantial amount of money.
Luckily, Dan was still healthy enough to pass health underwriting when he retired, and he enrolled in the plan of his choice with our help. However, we have seen many other retirees not be as lucky when they let their Medigap OEP lapse. Use Dan as a reminder that you should always be confident in WHY you are enrolling in Part B of Medicare, to keep all your Medigap options open. If you are concerned about being subject to a Part B penalty and your friends are saying, “you should sign up for Part B now that you are 65,” make sure you take 5 minutes to reach out to one of our advisors to compare all your coverage options. One quick phone call is all it takes to avoid an unnecessary and potentially costly mistake!
The Medigap Open Enrollment Period (OEP) is the 6-month period that begins on the first day of the month that you are BOTH 65 or older AND enrolled in Medicare Part B. Your Medigap OEP is unique to you, the individual and does not occur again, once it lapses. This should not be confused with the Annual Election Period (AEP) from October 15th – December 7th (which happens for all consumers enrolled in Medicare).
In Dan’s case, his Medigap Open Enrollment began the month he turned 65 (because he chose to enroll in Part B) and ended six months later, even though he never enrolled in a Medigap plan. That 6-month window was Dan’s opportunity to enroll in any Medigap plan he was eligible for in the Metro Detroit area, without health questions or the possibility of being denied coverage due to pre-existing conditions. Now, Dan was forced to either qualify for a Medigap plan through health underwriting or choose from a more limited amount of plans using his guarantee issue rights(learn more HERE)
The reason we use Dan as a case study is that his situation was 100% avoidable. He was covered by creditable health insurance provided by his large employer (over 20 employees), meaning that he was not at risk for a Part B penalty if he chose to delay his enrollment until his later retirement that he was planning.
In addition, to be an avoidable mistake, this is ended up costing Dan thousands of dollars of mostly unnecessary Part B premium. Because Dan’s employer had over 20 employees, it was the primary payer compared to Medicare. Having coverage through his employer meant that Medicare Part B premiums for secondary insurance that he was hardly utilizing since he is relatively healthy and rarely visited the doctors. As you may already know, the base rate for Medicare Part B in 2020 is $144.60/month. Over five years, this adds up to be a substantial amount of money.
Luckily, Dan was still healthy enough to pass health underwriting when he retired, and he enrolled in the plan of his choice with our help. However, we have seen many other retirees not be as lucky when they let their Medigap OEP lapse. Use Dan as a reminder that you should always be confident in WHY you are enrolling in Part B of Medicare, to keep all your Medigap options open. If you are concerned about being subject to a Part B penalty and your friends are saying, “you should sign up for Part B now that you are 65,” make sure you take 5 minutes to reach out to one of our advisors to compare all your coverage options. One quick phone call is all it takes to avoid an unnecessary and potentially costly mistake!
Fill out the form here and someone will be in touch soon.